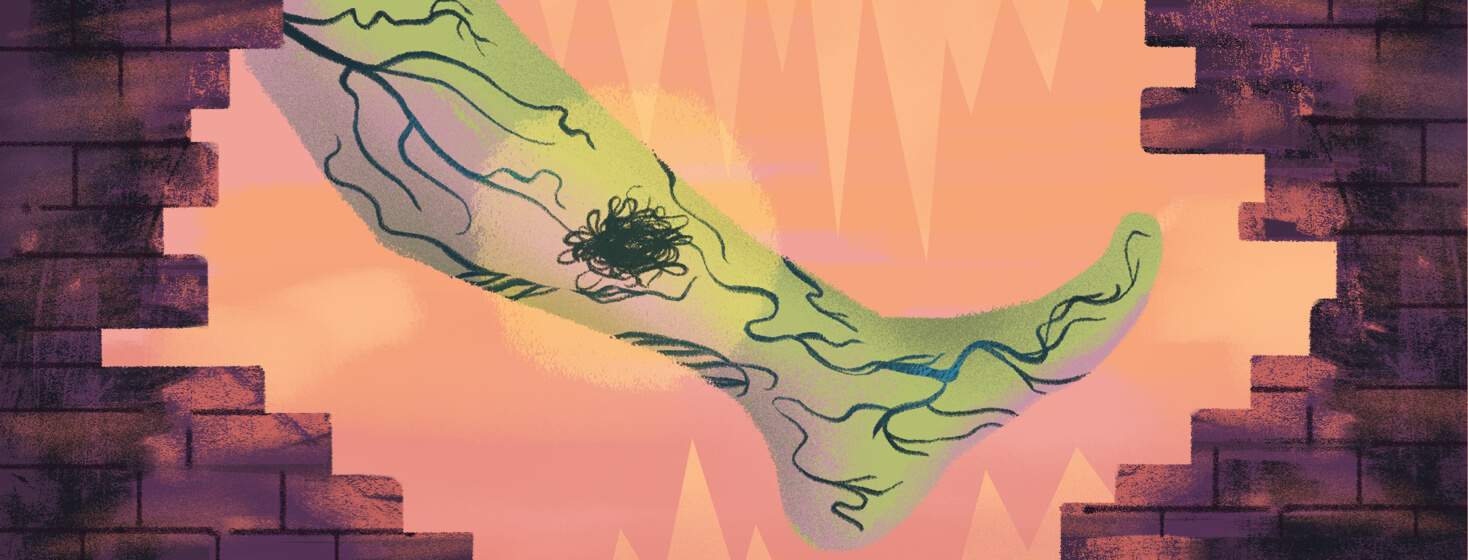
What Is DVT (Deep Vein Thrombosis)?
A deep vein thrombosis (DVT) is a blood clot, also called a thrombus. It can develop inside the deep veins of the body.1-2 These clots generally form in the lower leg or thigh but can form in other places.1 DVT can develop for many reasons and can go away on its own and be harmless. But if a part of the blood clot in a DVT breaks loose it can cause a serious problem.2 This is known as a pulmonary embolism (PE). It is caused by a blockage in one of the pulmonary arteries of the lungs that happens when a piece of the clot breaks away from the DVT and travels from the legs through the bloodstream to the lungs.
DVT statistics
A kind of venous thromboembolism (VTE), DVTs can develop in as many as 1 in 1,000 people and is a contributing cause of death for 60,000-100,000 people per year.1,3 It follows a heart attack and stroke as the third most common cause of death from cardiovascular disease.1 We don’t really know how often DVTs develop because the condition frequently goes undiagnosed. DVTs can cause pain or swelling, but also be present without any symptoms. When the symptoms are “silent”, there is often no treatment.1
Who gets DVTs?
Blood clots can be caused by immobility, certain medications, or conditions that affect the way blood clots including inherited conditions or an injury to veins or nearby tissue.2,4-5 Sitting still for a long time, whether at your desk all day, traveling in a car or airplane, or lying in a hospital bed can increase your risk for blood clots.2,4 They can also develop as a complication from surgery.1
DVTs can happen if the blood in a deep vein does not circulate or clot normally.4 The danger comes when part of a clot breaks loose as it can travel through the bloodstream and get stuck in the lungs. This can block blood flow, affect how the blood gets replenished with oxygen, and cause death.4 But DVT can be a largely preventable condition if people are educated about what to look for and how to lower their risk.3
DVT risk factors
People commonly at risk for DVT include those with cancer, congestive heart failure, obstructive airway disease, who just had surgery, or those who smoke. Obesity, pregnancy, and age- people over 60 are also at increased risk of developing DVT.1
There are 3 main categories of DVT risk factors, called Virchow's Triad:1,3
- Venous stasis – reduced blood flow due to extended bed rest, general anesthesia, surgery, stroke, or long-haul flights
- Vascular injury - damage to the blood vessel wall caused by trauma, surgery, IV drug abuse, or previous DVT
- Hypercoagulability – increased risk of clotting due to medical condition or genetics
Diagnosing DVT
Doctors use different tools to determine risk and diagnose a DVT.1 A physical exam and history (clinical), blood tests (biochemical), and imaging tests, most often ultrasound, are used to diagnose DVT.3 DVTs most often form below the knee in a deep or hidden area often with decreased blood flow.1,3 People with a DVT sometimes complain of pain or tenderness in the DVT area, especially when the foot is flexed. Others may experience swelling or redness. These are things your healthcare team will look for in examining you.1 The typical blood test used to indicate the presence of a DVT is called a D-dimer. It measures a protein that is a strong indicator of DVT but cannot identify the location of a clot. Ultrasound imaging is used to see deep into the veins and locate the specific clot.
Treating DVT
DVT can cause complications. The goal of DVT treatment is to prevent these complications; including pulmonary embolism, reducing the rate of death, and preventing or minimizing the risk of bleeding or developing post-thrombotic syndrome. Anticoagulation therapy, blood thinning, is the most common treatment for DVT.1,3 These are medicines that help to thin the blood, so it isn’t as sticky and doesn’t clot as easily. Other recommendations for managing DVT include getting up and walking, wearing compression stockings, and quitting smoking if you are a smoker.1
Join the conversation