Diagnosing Heart Failure
Reviewed by: HU Medical Review Board | Last reviewed: November 2019 | Last updated: March 2024
The European Society of Cardiology defines heart failure (HF) as a “clinical syndrome characterized by typical symptoms (e.g. breathlessness, ankle swelling, and fatigue) that may be accompanied by signs (e.g. elevated jugular venous pressure, pulmonary crackles, and peripheral edema) caused by a structural and/or functional cardiac abnormality, resulting in a reduced cardiac output and/or elevated intracardiac pressures at rest or during stress.”1 This is consistent with the definition used in the US as defined by the American Heart Association.
Defintions and symptoms of heart failure
These definitions of HF generally apply to the stages at which clinical symptoms are present and can be classified by either the New York Heart Association (NYHA) functional classification system or the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) classification which describes stages of HF based on structural changes and symptoms.”2
Sometimes symptoms are nonspecific, making it unclear if there is heart failure or another medical condition.1 If HF is suspected, the first step in the diagnostic evaluation is a thorough clinical history and a physical exam. These results combined with blood tests will provide an indication of whether further testing is required. If all are normal, it may prompt the physician to look for other causes; if an EKG is abnormal it may suggest moving on to other tests, such as an echocardiogram to further evaluate heart function.”1
Clinical recognition can be challenging
Clinical recognition of HF can be challenging, especially for primary care providers.2 The diagnostic criteria for evaluating heart failure are based on parameters established by clinical experts. There are guidelines established to facilitate the decision making of providers in their routine practice. The guidelines provide up to date clinical information that can help in the diagnosis and treatment of patients with heart failure. Ultimately, decisions on individual patient care are made by the patient and their provider.”1
Since the 1970’s, multiple sets of diagnostic criteria have been developed with varying sensitivities. The Framingham, Duke, Gothenburg, ESC, and Boston criteria were established before noninvasive techniques for assessing systolic and diastolic dysfunction became widely available. The criteria were designed to assist in the diagnosis of heart failure. All of these criteria have proven helpful in guiding healthcare providers, particularly in diagnosing advanced or severe heart failure.”4 Today, the Boston criteria are considered preferable when making a diagnosis of heart failure.”5
Boston criteria
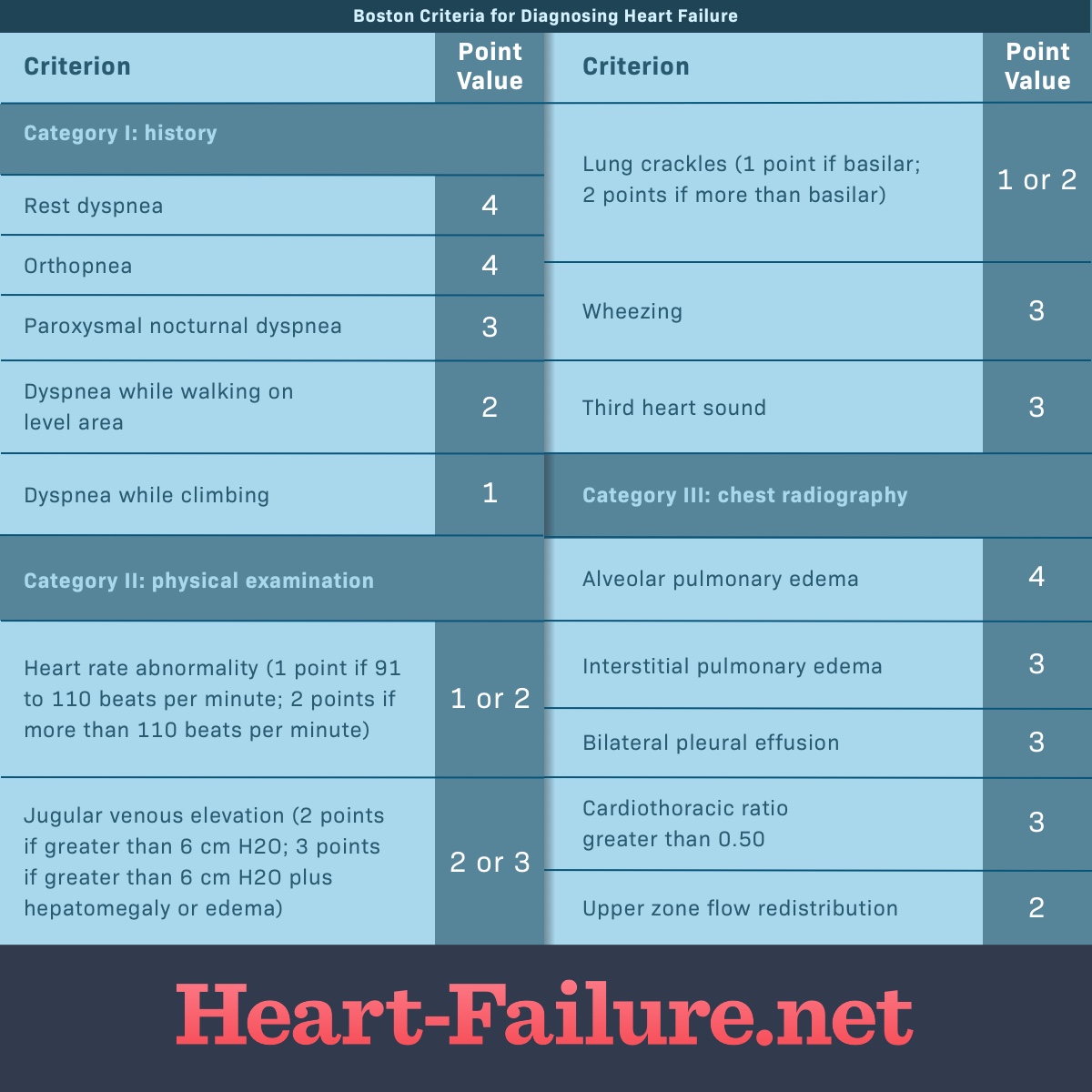
The chart below illustrates a points system based on symptoms. Up to 4 points can be counted from each of the three categories below. Added together they create a composite score with a maximum of 12 points. The diagnosis of heart failure is classified as “definite” at a score of 8 to 12 points, “possible” at a score of 5 to 7 points, and “unlikely” at a score of 4 points or less.”4-6
Figure 1. Boston Criteria for Diagnosing Heart Failure
Framingham criteria
The Framingham Heart Failure Diagnostic Criteria were developed in 1971 based on data collected during the Framingham Heart Study.”5 The Framingham Study breaks down symptoms of heart failure into major and minor criteria. To make a diagnosis of HF, a person must have 2 or more major criteria or 1 major criterion plus 2 minor criteria.4
Major criteria
The Framingham major criteria include:4
- Acute pulmonary edema
- Cardiomegaly
- Hepatojugular reflux
- Neck vein distention
- Orthopnea
- Pulmonary rales
- Third heart sound (S3 gallop rhythm)
- Weight loss >4.5 kg in 5 days in response to treatment
Minor criteria
The Framingham minor criteria include:4
- Ankle edema
- Dyspnea on exertion
- Hepatomegaly
- Nocturnal cough
- Pleural effusion
- Tachycardia (HR >120)