6-1/2 Years and Doing Pretty Well: What's Worked For Me
Sorry, this is a long one. This is my story.
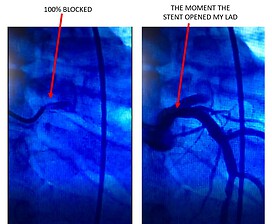
In 2016 at age 62, I had a massive heart attack with 100% blockage of my LAD (the Windowmaker) while traveling on business in a small town in Alabama. Because of unlucky circumstances, it was over 20 hours after the onset before I received one stent that saved my life.
I was in the ICU for 5 days, with my severely damaged heart, resulting in an ejection fraction of 20% and heart failure. I almost died and was terrified. Here I was, with heart disease, dilated cardiomyopathy, and heart failure because I was stressed, obese, sedentary, had sleep apnea (and did not use my CPAP machine), and ate too much salt. I wasn’t paying attention.
A surprising amount of sodium
As soon as I got out of the ICU and back home to Raleigh, NC, I completely changed my diet and lifestyle. I thought I had been eating a healthy diet. I ate lots of salads, fish and poultry, but I just plain ate too much, and too much of it was processed.
I added up my daily sodium intake from the canned fish on my salads, bottled salad dressing, whole wheat bread, and pre-cooked turkey breasts from Costco. I ate no beef, no hotdogs, no burgers. If I had fast food, it was a Chick-Fil-A salad. I was shocked to find that my daily sodium intake was around 6000 mg/day.
The processed foods were loaded with salt. Restaurant food was loaded with salt. Foods I never suspected had too much salt, such as bread, bottled salad dressings, cereal, and condiments. I immediately cut out all processed food and stopped going out to eat except for rare occasions. If we went out to eat, I would usually eat something at home before going to the restaurant, and then have only a salad.
Lifestyle and diet overhaul
I completely changed my diet and lifestyle. I kept a food log of what I ate every day with the calories and sodium content. I used the MyFitnessPal website to do this. Over the next six months, I lost 55 lbs. I also went through cardiac rehab and now go to a cardiac maintenance exercise program three times per week.
With heart failure, fluid retention and edema are the enemies and weight gain is the canary in the coal mine for worsening heart failure from fluid retention. Salt causes fluid retention, so I keep my sodium intake in the 1000-1500mg range per day. I also follow the Ornish diet, which is very low-fat, largely vegan, and with a little dairy allowed. Six years later, I still follow it.
The DASH diet and the Mediterranean Diet are also heart-healthy diets, but I have to be particularly focused on what I eat because of my past heart attack, and I choose to adhere to the stricter, very-low-fat Ornish Diet.
Long-COVID complications
So, it’s been over six and a half years since my heart attack. I have been largely asymptomatic with my heart failure, although I had a mild case of COVID-19 in early October 2022 (I am double vaxxed and double boosted).
I continue to have some long-COVID problems. I have developed some possible heart rhythm problems since I had COVID-19, and I wore a heart monitor for the month of November 2022. I’ll be discussing that with my electrophysiologist in mid-December.
In early December I had an echocardiogram to check for COVID-induced myocarditis and fortunately, I did not have that complication. My ejection fraction (EF) is only 30-35% and will likely not ever recover beyond that because of the structural damage to my heart from the heart attack.
Because my EF is below 35%, I am much more susceptible to going into cardiac arrest, so I have an implanted defibrillator as a protective measure. I have had this device for six years and so far, it has never zapped me, but I am glad I have it in case I need to be zapped.
Learning my limitations
Everyone is different. There are people with significantly better EFs than mine who have significant heart failure symptoms that they deal with daily. And then there are people, like me, with lower EFs who function pretty well.
My main limitation has been with strenuous aerobic activity. I do fine with moderate activity, but I run out of gas quickly with vigorous activity. This is because my weak heart cannot provide enough oxygenated blood to my muscles when they are subjected to strenuous aerobic activity, like running.
Up until my COVID issues, I could do physical work on my property all day long with no problem, and I’m hoping that my long-COVID symptoms will subside over time. I do now get tired in the late afternoon, even If I am not physically active, which was not the case before I contracted COVID-19.
I'm an A+ patient
I believe that in my case, a big reason that I have been largely asymptomatic with my heart failure is that I do what I am supposed to do as a patient. I take my meds religiously. I exercise. I eat properly. I get plenty of sleep. I now use my CPAP machine EVERY night. I keep my weight down. I take my heart failure very seriously.
Additionally, I have tried to educate myself as much as possible about my condition. I’m not talking about Facebook or other patient forums, though I have gotten some occasional good nuggets of information from them. I am talking about authoritative sources: Harvard, Mayo, NIH, PubMed, American College of Cardiology, AHA, JAMA Cardiology, Medscape, Cleveland Clinic, and Journal of Cardiac Failure.
I get weekly and monthly cardiovascular disease and heart failure-related feeds from some of these sources in my email. I even get medical continuing education lectures and presentations that are intended for physicians and medical professionals.
When I listen to these lectures, there is plenty I don’t understand about biochemistry and statistical analysis methods, but I stop the lectures and look up the meanings of terminology, acronyms, and abbreviations that I don’t know or don’t understand, and I gradually become more knowledgeable about the details of heart disease and heart failure.
I can ask informed questions of my cardiology team and gain a better understanding of my condition. These references also keep me quite up to date on the latest developments with heart failure drugs. There are great drugs for heart failure patients.
What I've learned and my advice about heart failure
Medications
With heart failure and dilated cardiomyopathy, your body secretes different enzymes, peptides and hormones that will try to make your heart beat harder to compensate for its diminished pumping capabilities, and that can be bad for your heart.
Back in 2016, when my heart failure was first diagnosed, the standard, core three-drug regimen for heart failure patients with reduced ejection fraction (my type) was a beta blocker, an ACE inhibitor, and a loop diuretic (“loop” refers to the loop of Henle, a structure in the kidney). ACE inhibitors mainly lower blood pressure by relaxing blood vessels in the body. Beta blockers mainly lower the heart rate, but they can also relax blood vessels.
My heart failure cardiologist explained that one important function of the beta-blocker is to slow the beating of my heart to permit my stiffer, damaged left ventricle more time to fill with blood before it’s pumped out to my body. The “blocker” and “inhibitor” labels refer to the fact that these drugs interrupt the function of hormones that would raise my blood pressure and make the damaged heart beat harder. These drugs take load off the heart.
Salt and Alcohol
Taking load off the heart is also a reason that a healthy, low sodium diet is important. Sodium makes your kidneys work harder, and the weakened heart cannot provide enough oxygenated blood to the kidneys to function properly. So, salt in your diet makes both your heart and your kidneys work harder.
Additionally, alcohol makes the liver work harder (and correspondingly, also the heart) so limiting alcohol is also important. I have, maybe, one drink per MONTH. The recommendations you will read in the literature online is a maximum of one drink per day for women and two drinks per day for men.
So, by eating a low-sodium diet, the kidneys do not have to work as hard. Knock on wood, both my kidney and liver functions remain normal. But as I said, I have at most one drink per month, and I keep my sodium (salt) intake to around 1000 mg per day.
New drugs for heart failure
There are some great new drugs for heart failure and two types of drugs that have been shown in recent large studies (PARADIGM-HF and DAPA-HF) to be particularly effective for heart failure with reduced ejection fraction (HFrEF). Those drug types are ARNI’s (angiotensin receptor/neprilysin inhibitors) and SGLT2 (Sodium-glucose Cotransporter-2) inhibitors.
You may have seen TV advertisements for them: Entresto (ARNI) and Jardiance and Farxiga (SGLT2 Inhibitors). In medical lectures I have listened to and from what my heart failure cardiologist has told me, the current evidence now suggests that patients with HFrEF should be treated early with a combination of four drugs: an ARNI, Beta-blocker, MRA (Aldosterone receptor antagonist – Spironolactone or Eplerenone), and an SGLT2 inhibitor.
Beta-blockers are cheap and MRA’s are cheap. Entresto and both Jardiance and Farxiga are not cheap, but their manufacturers do have financial assistance programs if you cannot afford them. They can work wonders and you need to ask your cardiologist about these drugs!
They can be hard on the kidneys, so if you have kidney disease, you may not be able to take these drugs, but you need to ask about them. A loop diuretic may be added to that list if you are retaining fluid and your cardiologist determines that you need to take a diuretic.
My daily log
One other important routine that I do daily is to take four readings and write them down in a daily log. I was told to begin this routine when I was in the hospital in Alabama, as soon as I was diagnosed with heart failure.
I created a log sheet in Microsoft Excel and have used it every day for six and a half years. It is part of my daily ritual and helps keep me engaged with my condition. It is a reminder, every day, to not blow off my diet; to not blow off my exercise; to be careful of my sodium intake.
Once a day is fine, but I personally do this twice a day, once in the morning and once before I go to bed. It’s in my face every morning and every evening. Here’s the routine:
Following my routine religiously
I weigh myself, take my blood pressure, and take my oxygen saturation level and heart rate. If you don’t do this but want to start, you should wear the same clothes or lack of clothes when you weigh yourself each day. First thing in the morning, when you get up is a good time to do it.
You can buy an inexpensive fingertip oximeter and a blood pressure cuff at CVS or Walgreens. Weighing yourself is very important. It is the first line of defense against fluid retention, which can be a serious problem for heart failure patients. If you begin retaining fluid, your cardiologist may prescribe a diuretic to shed fluid.
I take a diuretic every day. When I first started this routine, If I gained three pounds or more in one day, or five pounds in one week, I was supposed to call my heart failure team so they could instruct me on taking additional diuretic pills to bleed off that excess fluid.
They have now trained me in how to manage this myself, so I do not need to call them if I start gaining weight, and I manage it myself. If, for some reason, I did not begin to shed fluid with the doses that I have been instructed to take, I would call the heart failure clinic for further instructions.
Grateful for my cardiology team
The last piece of advice I want to give is that you MUST be your own advocate! If you are not getting what you need from your cardiologist, tell them, and if they still do not give you what you need in that regard, look for a new cardiologist.
I actually have three cardiologists, and my cardiology team is fantastic. I have an interventional cardiologist who deals with my cardiovascular disease and heart attack-related issues. He is my “plumber." I have an electrophysiologist, who is the cardiologist who deals with my heart’s electrical issues and my defibrillator, and I have a heart failure cardiologist with a full heart failure clinic team behind him.
Finding the right healthcare team for you
My heart disease is pretty well controlled, and my heart failure is the biggest issue I deal with, and so my heart failure team is now my first point of contact. Heart failure clinics are experts in designing treatment programs unique to each patient. They are particularly adept at dialing in the right combination of drugs to maximize their effectiveness on each patient.
Heart failure clinics are not always available in smaller towns and cities. They are often associated with a hospital with a cardiology department. However, I cannot emphasize enough how important my heart failure clinic has been to the stability of my heart failure and my quality of life.
If your cardiologist is not a heart failure specialist, ask your cardiologist to refer you to a heart failure specialist and/or heart failure clinic, if at all possible.
Five hospitalizations later...
In the first year of my heart attack, I was hospitalized five times. The first hospitalization was when I had my heart attack and was in the ICU for one week. The second hospitalization was four months later when I was hospitalized for acute (decompensated) heart failure with a pleural effusion.
Up until then, my cardiology team did not include a heart failure specialist or the heart failure clinic. The focus was on preventing me from having another heart attack. But with this episode, my heart failure moved to the top of the priority list. I got a heart failure specialist and deluxe membership to the heart failure clinic out of that deal!
The third hospitalization was four months later with the implantation of my defibrillator. The fourth hospitalization was two months later for a procedure called a talc pleurodesis, during which one of my lungs had to be collapsed to permanently fix a recurrence of my pleural effusion.
Finally, the fifth hospitalization was for a chest pain scare that proved to be a false alarm. All during this time, my cardiology team was working to stabilize my condition, get my drug regimen dialed in, and address new problems that cropped up as a result of my cardiovascular disease and heart failure.
They did a great job. I have had no hospitalizations since then. It’s now been over five years. There are a few activities I enjoyed that I now can’t do because of my heart failure (SCUBA diving, is one), but that’s OK. My quality of life is good and I’m very grateful to be alive.
Do you have a heart failure story? Click the button below to share with our community!
Join the conversation